Understanding Mitral Valve Regurgitation
Mitral valve regurgitation is when the mitral valve in the heart is leaky. It lets some blood flow backward when the ventricle squeezes.
How mitral valve regurgitation happens
The mitral valve is one of the heart’s four valves. Normally, these valves close tightly to help the blood flow through the heart’s four chambers and out to the body. Each valve has a set of flaps (leaflets or cusps) that open and close with every heartbeat. The flaps make sure blood flows in the correct direction.
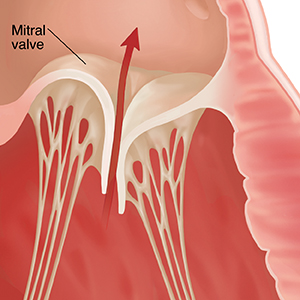
The mitral valve lies between the left atrium and the left ventricle. It has two flaps. Normally, the mitral valve stops blood from flowing back into the left atrium from the left ventricle when the ventricle squeezes. This maximizes forward blood flow through the heart and out to the body.
With mitral valve regurgitation, the valve doesn't close tightly. Some blood leaks back through the valve instead of flowing forward through the heart or into an artery. As some blood flows in the wrong direction, your heart cannot work efficiently to send oxygen-rich blood to your body. When this blood is regurgitated backward in the heart, it causes the heart to pump harder and increases the pressure within the heart. This can lead to muscle damage as well as high blood pressure in the lungs.
Mitral valve regurgitation can increase the risk for other heart rhythm problems, such as atrial fibrillation (AFib). This abnormal heart rhythm results in fast and irregular heartbeats. AFib can also lower the heart's pumping ability and increase the risk for stroke.
Mitral valve regurgitation can be acute or chronic. If it’s acute, the valve suddenly becomes leaky. In this case, the heart doesn’t have time to adapt to the leak in the valve. Symptoms are often severe. If you have severe mitral valve regurgitation, you may need a catheter procedure or surgery to repair or replace the leaking valve.
If it’s chronic, the valve leaks more and more over time. The heart and the body have time to adapt to the leak.
What causes mitral valve regurgitation?
Mitral valve regurgitation can be caused by various things, such as:
-
Heart attack or coronary artery disease.
-
Natural aging that can damage the mitral valve.
-
Tearing of the tissue or muscle that supports the mitral valve, sometimes due to an injury.
-
Floppy mitral valve (mitral valve prolapse).
-
Rheumatic heart disease from untreated Streptococcus (strep) infection. Strep are the bacteria that cause strep throat.
-
Certain autoimmune diseases, such as rheumatoid arthritis.
-
Infection of the heart valves.
-
Heart problems present at birth.
-
Certain medicines. These include weight loss medicines that were used to treat obesity (fen-phen), anti-migraine medicines such as ergotamine and methysergide, and drugs like MDMA (ecstasy).
You can reduce some risk factors for mitral valve regurgitation. For example, you can:
-
Use antibiotics as directed to treat a strep infection and prevent rheumatic heart disease.
-
Reduce the risk of heart valve infection by not injecting illegal drugs.
-
Manage risk factors that can lead to a heart attack or chronic heart artery disease.
There are other risk factors that you can’t change. For example, some conditions that can lead to mitral valve regurgitation are partly genetic.
Symptoms of mitral valve regurgitation
Chronic mitral valve regurgitation often doesn’t cause symptoms for a long time. Mild or moderate mitral valve regurgitation often doesn’t cause any symptoms. If the condition becomes more severe, you may have symptoms. They may get worse and happen more often over time. Symptoms may include:
-
Shortness of breath with physical activity.
-
Shortness of breath when lying flat.
-
Feeling tired.
-
Less ability to exercise.
-
Awareness of your heartbeat, such as feeling a pounding in your chest (palpitations) or racing and irregular heartbeats that accompany AFib.
-
Swelling in your legs, abdomen, and the veins in your neck.
-
Chest pain (less common).
Acute, severe mitral valve regurgitation is a medical emergency that can cause serious symptoms such as:
-
Symptoms of shock (pale skin, loss of consciousness, rapid breathing).
-
Severe shortness of breath.
-
Cough with clear or pink, frothy sputum (mucus).
-
Arrhythmias (abnormal heart rhythms) that make the heart unable to pump blood well.
Diagnosing mitral valve regurgitation
Your health care provider will ask about your health history. They will give you a physical exam. Using a stethoscope, your provider will listen to your heart. This is to check for sounds called heart murmurs and other signs that the heart isn’t pumping normally. You may also have tests such as:
-
Echocardiogram, to look at the structure and function of the heart using sound waves.
-
Stress echocardiogram, to see how well the heart functions during exercise.
-
Electrocardiogram (ECG), to check the heart’s rhythm.
-
Cardiac MRI, transesophageal echocardiogram, or cardiac catheterization, if more information is needed.