Having a Septal Myectomy
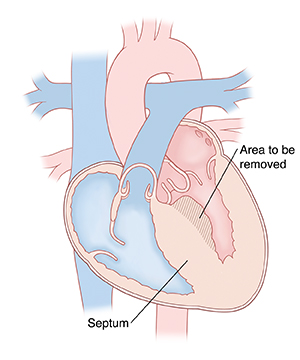
Septal myectomy is a type of open-heart surgery. It’s done to treat hypertrophic cardiomyopathy. This is when the heart muscle becomes thick. During the surgery, extra muscle is removed from the septum. The septum is a wall that separates the left and right sides of the heart. This lets the blood pump through the heart more easily.
What to tell your healthcare provider
Before your surgery, tell your healthcare provider:
-
What medicines you take. This includes prescription and over-the-counter medicines (such as ibuprofen). It also includes vitamins, herbs, and other supplements. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin.
-
If you smoke. You may need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
-
If you’ve had recent changes in your health. This includes an infection or fever.
-
If you are sensitive or allergic to anything. This includes medicines, latex, tape, and anesthetic medicines.
-
If you are pregnant. Also tell your healthcare provider if you think you are or could be pregnant.
Getting ready for your surgery
Make sure to do the following:
-
Ask a family member or friend to take you home from the hospital
-
Make plans for some help at home while you recover
-
Follow all other instructions from your healthcare provider
-
Read the consent form and ask questions if something is not clear
-
Follow any directions you are given for not eating or drinking before surgery
Tests before your surgery
Before your surgery, you may need tests, such as:
-
Chest X-ray
-
Electrocardiogram (ECG), to check the heart rhythm
-
Blood tests, to check your general health
-
Echocardiogram (ultrasound), to look at your heart and blood flow through your heart
-
Heart catheterization, to look at the coronary blood vessels
On the day of your surgery
Your procedure will be done by a heart surgeon. They will work with a team of specialized nurses. The surgery can be done in several ways. Ask your healthcare provider about the details of your surgery. The whole procedure may take several hours. In general, you can expect the following:
-
You will have general anesthesia, a medicine that allows you to sleep through the surgery. You won’t feel any pain during the surgery.
-
A healthcare provider will watch your heart rate, blood pressure, and other vital signs during the surgery. You may have a breathing tube put down your throat during the surgery to help you breathe.
-
Hair in the area of the surgery may be removed.
-
The surgeon will make an incision down the middle of your chest. Part of your breastbone will be separated.
-
The surgery team will attach you to a heart-lung machine. This machine will provide oxygen to your blood and pump the blood to your body during your surgery.
-
The surgeon will cut away part of your thickened septum.
-
The surgery team will remove the heart-lung machine.
-
They will wire your breastbone back together.
-
The team will close the incision in your skin with stitches or staples. A bandage will be put on the area.
After your surgery
After the procedure, you will spend several hours in a recovery room. You may be sleepy and confused when you wake up. Your healthcare team will watch your heart rate, breathing, and other vital signs. You may have a tube in your throat to help you breathe. This may be uncomfortable, and you won’t be able to talk. The tube will likely be removed within 24 hours. You will likely have a tube draining the fluid from your chest. You may feel some soreness, but you shouldn’t feel severe pain. You’ll be given pain medicine if you need it.
Your symptoms of hypertrophic cardiomyopathy should get better right away. You will likely be in the hospital for about 5 days. You will likely be able to drink fluids the day after surgery. You can have regular food as soon as you are able. In 1 to 2 days, you should be able to sit in a chair and walk with help. You may do breathing therapy. This is to help remove fluid that collects in the lungs during surgery. You may need to wear compression stockings. These are to help blood flow through your leg veins.
Recovering at home
Make sure you have someone to drive you home from the hospital. You will also need help at home while you recover. You may tire easily after the surgery. You will recover your strength over time. Recovery time varies, but it will be at least several weeks. As you recover:
-
Follow all the directions your healthcare provider gives you for medicines, exercise, diet, and wound care.
-
Take your temperature and check your weight every day.
-
Ask your healthcare provider when it is safe for you to drive.
-
Ask your healthcare provider what is safe for you to lift. Don’t lift anything heavy for several weeks.
Follow-up care
You will probably have your stitches or staples removed in a follow-up appointment in 7 to 10 days. Be sure to keep all follow-up appointments.
When to call your healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Fever of 100.4°F ( 38°C) or higher, or as directed by your healthcare provider
-
Sudden change in your weight
-
Clicking or movement of your breastbone
-
Fluid leaking from your incision
-
Swelling of the legs or abdomen (belly)
Call 911
Call 911 if any of the following occur:
-
Fast, slow, or irregular heartbeat
-
Chest pain that gets worse, or unusual chest pain
-
Difficulty breathing that is new or gets worse
-
Dizziness or fainting